Binal, a 27-year-old marketing professional, tells me during a therapy session that she hasn’t stopped crying for three weeks, has been feeling extremely hopeless, and a deep sense of melancholy has been eating her up from within. A well-paying job and a supportive partner don’t seem to matter anymore, and she wonders whether there is any point in living. Even getting out of bed takes an effort, and she is chronically fatigued, she says. “Do you think I’m depressed?” she asks me, tears in her eyes. Raman, a 40-year-old businessman, married with two children, tells me that a sense of darkness has consumed him for the past few months. All day long, he feels a sharp twinge of sadness that doesn’t allow him to think or function. He tells me he hasn’t been sleeping and has lost about three kilograms in two weeks. “I don’t want to die really, but I wish something happens to me so that I can escape this misery,” he says. Both Binal and Raman suffer from clinical depression. What do you think the health ministry, the highest nodal body that regulates health-related issues in the country, would have them do to deal with their depression? According to the Ministry of Health and Family Welfare, one must take up activities “that keep him or her boosted in order to cope with depression”. The ministry on Thursday took to Twitter to say : “Depression is a state of low mood that affects a person’s thought, behaviour, feeling and sense of well-being.” This was followed by tips such as yoga, taking multivitamins, being creative, etc, as ways to deal with depression.
#Depression is a state of low mood that affects a person's thought, behaviour, feeling & sense of well-being. One must take up activities that keep him or her boosted in order to cope with depression. #SwasthaBharat #MentalHealth #LetsTalk pic.twitter.com/UJR3X7GwL2
— Ministry of Health (@MoHFW_INDIA) June 26, 2018
From a mental health perspective, this definition and the tips are not just inaccurate, but also add to the already existing misconceptions about depression. The poster doesn’t even acknowledge the need for a psychiatrist or psychologist to deal with depression. According to the World Health Organisation (WHO), depression is the world’s leading cause of disability, and it estimates that over 300 million people worldwide suffer from the illness. Moreover, the advice the poster gives — “think positive, be creative, follow a routine, travel” — does not help at all. Narratives like these trivialise a concern like depression and also make the person feel small, incompetent and guilty about what they are feeling and are helpless against. Most people struggling with depression find it hard to even attend to their daily hygiene. That’s how foggy they feel in their head (so positive thoughts can’t work at all), while multivitamins are not a solution to depression. The health ministry’s tweet, unsurprisingly, was criticised by several quarters , including experts, those who suffer from depression as well as those who have seen their loved ones try to fight the illness. An organisation that provides help to mental health patients found it necessary to point out how wrong the ministry was: “People with depression can’t think positive. That’s the definition of depression.” The advice given by the health ministry is damaging to all of us — the patients and caregivers alike. It derails all the hard work that has been done to deal with the societal stigma around mental health. Depression comes under the category of mood disorders and requires a more nuanced, research-based intervention to treat it. What constitutes depression? Depression is not being low or being in a sad mood; there is a huge difference between the two. We all experience sadness in our day-to-day life, with a bad day at work, a tiff with a partner, or sometimes even regarding our own choices. Having said that, sadness is a more transient feeling and is not all-consuming. Depression, on the other hand, impacts every realm of our being and functionality. It is more persistent and can exist in the absence of a negative or stressful life event. To use an analogy from Harry Potter to describe what depression feels like: It’s like the dementors have sucked out your soul and all your energy, leaving you with nothing to hold on to, while everything feels meaningless and futile. According to the Diagnostic and Statistical Manual of Mental Disorders, published by the American Psychiatric Association, the criteria for clinical depression includes being in a depressed mood and loss of interest or pleasure (anhedonia). These two symptoms need to be accompanied by five or more symptoms for a two-week period and also show that there has been change from the individual’s previous state. - Fatigue or loss of energy nearly every day - Significant weight loss or weight gain (change in appetite) - Insomnia or hypersomnia nearly every day - Excessive guilt, feelings of worthlessness - Diminished ability to think/concentrate - Suicidal ideation/recurrent thoughts of death - Psychomotor retardation or agitation nearly every day Depression can be caused by a multitude of factors, which include genetic history, role of neurotransmitters and psycho-social factors. Certain personality factors that which predispose an individual to depression also take a toll on them. What does dealing with depression mean? Depression responds well to a combination of psychotherapy and psychiatric medication. Research shows that the treatment is quite effective, though the number of people who receive help worldwide, or even receive diagnosis, is still an area that needs discussion. [caption id=“attachment_4637071” align=“alignleft” width=“380”] 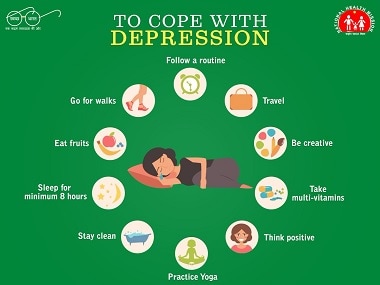 The tweet sent out by the health ministry. Courtesy: Twitter/@MoHFW_INDIA[/caption] However, in my understanding, the responsibility of dealing with depression lies not just with the individual, but with the society at large. We need to develop resilience at the macro level to ensure that individuals feel safe to acknowledge their mental health concerns to begin with. The government’s poster has just negated that belief in the machinery at large and trivialised the deep emotional pain of so many struggling with depression. We, as a nation, can become resilient only when we can work towards integrating structural policies in consultation with mental health professionals, which address the concerns of people in rural and urban areas. The narrative of accountability and availability of mental health professionals is what the government needs to address when it comes to mental health. Dixon Chibanda, a Zimbabwe-based psychiatrist, talks about the Friendship Bench Project in his TED Talk, where he trained grandmothers in evidence-based talk therapy (cognitive behavioural therapy), and his documentation show how powerful the healing experience has been. He felt that in a nation like theirs, this was an effective way to provide access and affordability and create awareness about mental health. We, as a nation, need more approaches like this, with peer counsellors, community workers, mental health professionals and solid policies that allow for timely intervention. At a micro level, our awareness about mental health, learning to look at the act of seeking help as a sign of strength and not a weakness is a good step. As parents, we need to educate our children about how mental health issues can be dealt with and managed, in turn allowing hope, breaking stigma and timely intervention. While passing the Mental Health Care Act was a step in the right direction, this is a moment for the government and all of us to reflect on how to create safe spaces that ensure understanding, awareness and empathy towards those struggling with mental health issues like depression. The author is a Mumbai-based practicing clinical psychologist who has worked in the field of mental health for 13 years.


)

)
)
)
)
)
)
)
)



