The recent Hindi movie, Judgementall Hai Kya?, exceeded expectations, and finally got us thinking of mental health in ways beyond prescribed stereotypes. As one goes deeper into the conversation on mental health, it might be a good time to reflect on whether we’ve understood it right. For example, what would you understand if someone told you that hundreds of people have congregated in a closed space, have painted their faces in different colours, are drinking alcohol, and are shouting and dancing? Probably a cult ritual? A wild drug party, maybe? Now, what if you are informed that these are spectators at a football match? Ah, that sets things into context, doesn’t it? As humans dealing with several emotional triggers on a regular basis – like exposure to early life trauma, unsafe circumstances in life, sexual abuse, bad parenting, job loss, economic despair, lack of acceptance due to a mental or physical disability, competitive environment, and climate crisis — is it surprising then, that depression, anxiety, and other mental health conditions are widespread? These phenomena are, therefore, better understood as reactions to events constantly unfurling around us. [caption id=“attachment_4955681” align=“alignnone” width=“825”]  Illustration by Satwik Gade[/caption] In his book Lost Connections, journalist Johann Hari explores how mental health symptoms are so much more common among oppressed races, the poor, women and other non-male genders, highlighting that those who are more disenfranchised in society, more unsafe or more ostracised, tend to show more symptoms of mental health disorders. A striking example from his book cites that more than 50% of the women from a weight control group that he surveyed had gone through sexual abuse. It was as if gaining weight was subconsciously or consciously a way of avoiding male attention, in an attempt to avoid further sexual abuse. Therefore, while from a medical viewpoint weight gain doesn’t help, the mind perceives it as a good way to ward off unwanted attention. In his TED talk on addiction, Johann Hari says, “The opposite of addiction is not sobriety, it’s meaningfulness.” According to his research, addiction is a way to deal with a life that doesn’t feel safe, meaningful or fulfilling. Released in the Journal of British Psychological Society in 2018, ‘The Power Threat Meaning Framework’ (PTM Framework) by Dr Lucy Johnstone and Dr Mary Boyle talks about the need for a framework that looks at mental health by going beyond symptoms. It attempts to assess people as functioning in response to the threats they feel, the meaning they make of these threats, and how they react to them. All of these factors are treated as coping mechanisms. Johnstone and Boyle believe that currently, mental health conventionally only locates the problem in the person, which is akin to saying that if pollen in the air makes you sneeze, then you are at fault for sneezing (instead of reading it as an interaction with the pollen). They feel that this perspective not only blames people for what is not their fault, but also fails to help them adequately, since their coping mechanisms are seen as ‘symptoms’, which are ‘bad’. This takes power away from the people, and puts it in the hand of the medical professional. Further, this means that the solutions are not driven by clients or patients, but by doctors. They do not cover the full range of solutions, and then stay limited to medication or changing one’s thoughts and feelings. Many symptoms of mental health disorders also require reconnecting with society and community, along with larger institutional changes — like job security, equality and safety – factors that are controlled by governments and similar agencies in society. Clearly, this entire conversation goes missing when an individual is held responsible for their reactions to circumstances and events. ‘The PTM Framework’ is highly empowering and useful to clients and professionals who can think of novel solutions to empower people on adapting to it. The framework centrally asks the following questions:
- What has happened to you? (How has Power operated in your life?)
- How did it affect you? (What kind of Threats does this pose?)
- What sense did you make of it? (What is the Meaning of these situations and experiences to you?)
- What did you have to do to survive? (What kinds of Threat Response are you using?)
When translated into practice with an individual, family, or group, two additional questions need to be asked:
- What are your strengths? (What access to Power resources do you have?)
- And to integrate all the above: What is your story?
The framework is not exactly new in its content — smaller attempts have been made to go for more holistic, survivor-led, non-medical understanding of mental health issues, but the PTM Framework does a good job of bringing all the work before it together, and becoming a powerful tool. The paper describes the kinds of threats people experience, as well as the aspects of these adversities that affect us. For example, long-lasting danger makes us feel trapped, and it affects our ability to trust our own intuitions and other people. Someone may cope with this by being vigilant, checking locks on doors multiple times, or by not trusting what people say. Without the context of what they went through, this might appear as “obsession”. [caption id=“attachment_7235661” align=“alignnone” width=“825”] 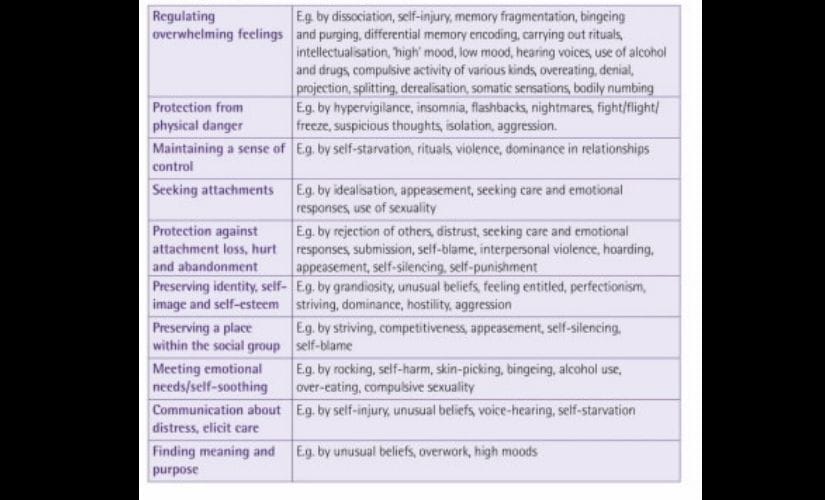 Threat responses, as grouped in ‘The Power Threat Meaning Framework’.[/caption] The paper then goes on to describe seven “functional patterns” in detail, which speak of major threats and threat responses that people may engage in. The seven patterns are as follows:
- Surviving certain identities (referring to marginalised people, certain gender groups, etc.)
- Surviving rejection, entrapment and invalidation
- Surviving disrupted attachments and adversities as a child/young person
- Surviving separation and identity confusion
- Surviving defeat, entrapment, disconnection and loss
- Surviving social exclusion, shame, and coercive power
- Surviving single threats (not as crippling as some of the other categories, but could still be devastating. For example, surviving a tsunami with the sense of loss could be tough)
The paper then suggests certain examples for interviewing clients that not only take into consideration their powerlessness and threat experiences, but also looks at their coping resources. The strengths that they displayed, — either as “symptoms” or other coping mechanism — or the sources of support around them, are then used to create an alternative paradigm of meaning, in order to help create a workable treatment plan. The study also cites examples of movements and groups that are survivor-led, and have been the inspirations for the PTM overview. One interesting example is “streetherapy” (street-therapy) — a way of working with at-risk young people that involves the use of casual games and conversations on the streets. Such programmes have been influential in keeping youngsters away from drug use, and out of jail. The current system of medicalisation and institutionalisation has many pitfalls — a limited understanding of the human condition, high relapse rate, high costs, high likelihood of abuse of power by the professionals involved, and lastly, lack of empowerment for the survivors. It also leads to a murky bifurcation of criminal and psychiatric behaviour issues. The report also suggests re-looking at the ways in which criminals are dealt with, and mentions certain programmes providing therapeutic help to first-time criminals. This leads to a significant improvement in them, in comparison to the results yielded by the punishment-led justice system. When India had no conversation on mental health, the comfort of clinical terms and medicalisation was helpful to at least get the ball rolling. But now is the time to make our understanding more nuanced. As mentioned in the ‘PTM Framework’, “Diagnosis has been shown, overall, to incline the person diagnosed to have less optimism about recovery, make less effort to recover, and be more likely to use alcohol to cope, as well as to have lower perceived control over their difficulties and undermining the effects of therapy.” ‘The PTM Framework’ is freely available for reading, in both short and long versions. It is an attempt to encourage mental health systems into adapting this framework in their lives and workplaces, in order to ease conversations on the issue.


)
)
)
)
)
)
)
)
)



