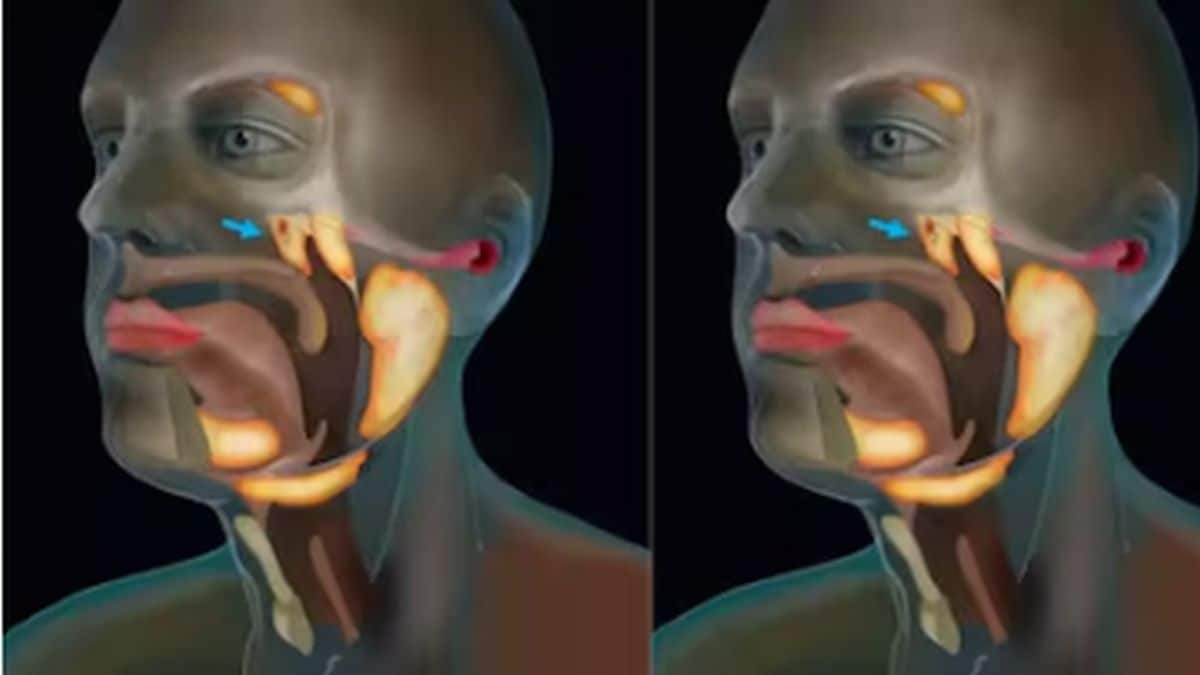
While there are many things we have learnt about SARS-CoV-2, the causative agent of COVID-19 disease, we still can’t say that we know exactly how our immune system reacts to the virus. Now a group of researchers at the University of Pennsylvania say that they have found two important things about the human immune system’s response to the virus. First of all, humans have three different immune reactions to the virus and these reactions are related to the disease severity. Secondly, distinct disturbances in the leukocytes (a type of white blood cell) mark severity of COVID-19. The two studies are published in the journal Science and Science Immunology, respectively. The three responses For the first study, a research team at the Penn Institute of Immunology analysed the immune response of 125 COVID-19 patients through the course of their sickness and compared it with samples from 36 recovered plasma donors and 60 healthy people. The median age of all the COVID-19 patients was 60, whereas the age of the recovered group was 29 and that of the healthy group was 41. However, people of overlapping age groups were found in all three groups. About 83 percent of all patients in the COVID-19 cohort had cardiovascular diseases and about 20 percent had chronic kidney disease. About 18 percent were immunocompromised and 7 percent had some sort of lung condition or cancer. About 30 percent patients required mechanical ventilation and at least four needed additional ECMO (extracorporeal membrane oxygenation). Three distinct immune types were found in all the patients that were then studied with the use of a system called Uniform Manifold Approximation and Projection (UMAP) to link them to disease severity:
- Those who had robust CD4 T cell activation, lack of cTfh (cells that stimulate B cell maturation) and lack of CD8 T cells: these people had severe disease including severe inflammation, organ damage, and acute kidney disease.
- More CD8 T cells, less CD4 T cells and memory B cells: this immunotype was not related with disease severity but mortality and pre-existing immunosuppression. These features were improved with the use of NSAIDs (non-steroidal anti-inflammatory drugs) and remdesivir.
- Those who had minimal lymphocyte activation: they failed to maintain a robust immune response against the virus. These people had less severe disease or didn’t show any link to any clinical features of the disease.
The study mentioned that the varying immune responses is why not all COVID-19 patients can fight the disease equally or in the same way. Explaining the importance of the study, Dr E John Wherry, senior author of the study, chair of the Department of Systems Pharmacology and Translational Therapeutics and director of the Penn Institute of Immunology, said in a news release that based on the clinical data, one may actually be able to predict or infer the kind of immune response a patient would have against the disease and this would be helpful in enrolling different types of patients in clinical trials investigating treatments. The second study About 42 COVID-19 patients with severe or moderate disease or those who had recovered were compared with 12 healthy individuals to study the changes in immune response and the relation of immune response to disease severity. Just like the previous study, heterogenous immune response was found with robust CD4 and CD8 cells, neutrophils, monocytes, B-cells and NK (natural killer) cells. Increase in neutrophil count along with reduction in lymphocytes was a biomarker of severe COVID-19 and organ failure. Neutrophils are white blood cells that fight infection by ingesting the pathogens. The number of neutrophils progressively increases during infections. Reduction in certain markers present on neutrophils and NK cells (another type of immune system cells that kill viruses) was also seen. This was believed to play a role in redistribution of both these cells to the lungs to fight the virus. However, more studies are needed to understand how these cells are contributing to the three immunotypes. Praising the findings of the research in a news release, Jonathan A Epstein, MD, executive vice dean, chief scientific officer and a professor of cardiovascular research at Penn University said, “The deep immune-profiling work the investigators applied here is likely to be useful not only now, for this disease, but into the future for many others.” For more information, read our article on Mild vs severe symptoms of COVID-19 Health articles in Firstpost are written by myUpchar.com, India’s first and biggest resource for verified medical information. At myUpchar, researchers and journalists work with doctors to bring you information on all things health.


)
)
)
)
)
)
)
)
)



