Throat cancer, once predominantly associated with tobacco and smoking is increasingly affecting non-smokers in India, particularly men under the age of 60. Medical experts are now sounding the alarm over a dramatic epidemiological shift, citing the human papillomavirus (HPV) as a key driver of this growing trend.
“Traditionally, oropharyngeal cancers in India were largely seen in smokers and tobacco chewers. But now, a growing number of patients, especially men in their 50s—are being diagnosed without any history of smoking,” said Dr Mandeep Singh Malhotra, Director of Surgical Oncology at CK Birla Hospital, Delhi.
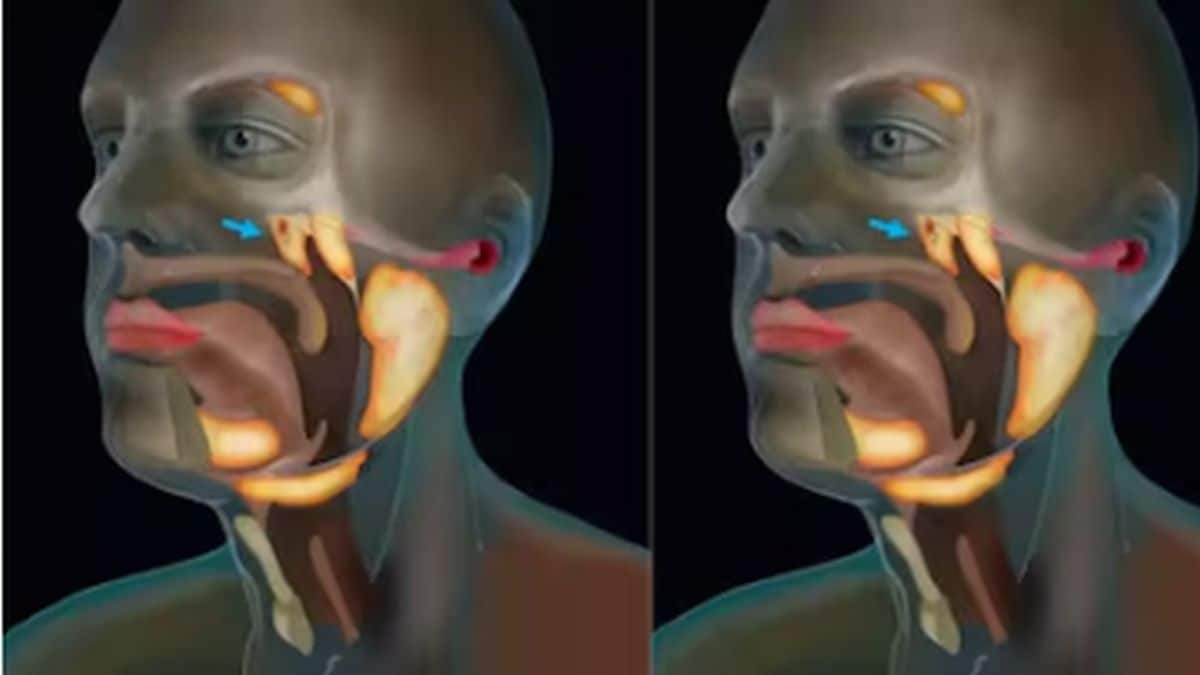
Dr Malhotra highlighted that areas most commonly affected include the tonsils, base of the tongue, posterior pharyngeal wall and tissues above the voice box.
HPV i****nfection the d****riving f****orce
The primary factor behind this shift, he said, is the rising incidence of HPV infections which are closely linked to changes in sexual behaviour. “Increased prevalence of oral sex compared to previous generations has led to higher exposure to HPV, a known carcinogen for the oropharynx,” Dr Malhotra said.
A 2023 study published in The Lancet Regional Health – Southeast Asia supports this, reporting that HPV-positive oropharyngeal cancers are on the rise in India, echoing trends observed in Western countries over the past two decades.
Other contributing factors include excessive alcohol consumption, poor oral hygiene, a diet low in antioxidants, vegetables and environmental exposure to petrochemicals, wood dust and industrial pollution.
Distinct b****iology and b****etter p****rognosis
HPV-related throat cancers are biologically different from those caused by tobacco, says Dr. Malhotra. “They tend to respond much better to chemotherapy and have a higher cure rate, even though they can present at more advanced stages with larger neck nodes. In contrast, cancers linked to smoking and alcohol are often more aggressive and harder to treat.”
A 2023 meta-analysis published in JAMA Oncology found that five-year survival rates for HPV-positive oropharyngeal cancer were above 80%, significantly better than the 50-60% rates seen in HPV-negative cases.
Breakthroughs in treatment: TORS and bio-Selection
Treatment advancements such as Transoral Robotic Surgery (TORS) have revolutionised outcomes, particularly for early-stage patients. “TORS is minimally invasive, leaves no external scars or bone cuts, and enables faster recovery,” he added.
For advanced cases, oncologists are now adopting a ‘bio-selection’ approach. Patients first receive 2–3 cycles of chemotherapy to assess tumour shrinkage. If the tumour reduces by 50–80%, less invasive options like TORS or radiation can be pursued. If not, a radical surgery followed by radiation becomes necessary.
Impact Shorts
More Shorts“This strategy allows us to personalise treatment based on tumour biology rather than a one-size-fits-all approach, ultimately reducing complications and improving survival outcomes,” said Dr Malhotra.
According to the Indian Council of Medical Research (ICMR), India sees over 1.3 lakh new cases of head and neck cancers annually, with oropharyngeal cancer forming a significant portion. Globally, WHO estimates that HPV is responsible for up to 70% of oropharyngeal cancers in developed countries, a number now reflecting similar patterns in India.
As the medical community adapts to these evolving patterns, awareness and early detection remain key. “Vaccination against HPV, improved oral hygiene and safe sexual practices are preventive strategies that must be prioritised,” Dr Malhotra said.


)
)
)
)
)
)
)
)
)



