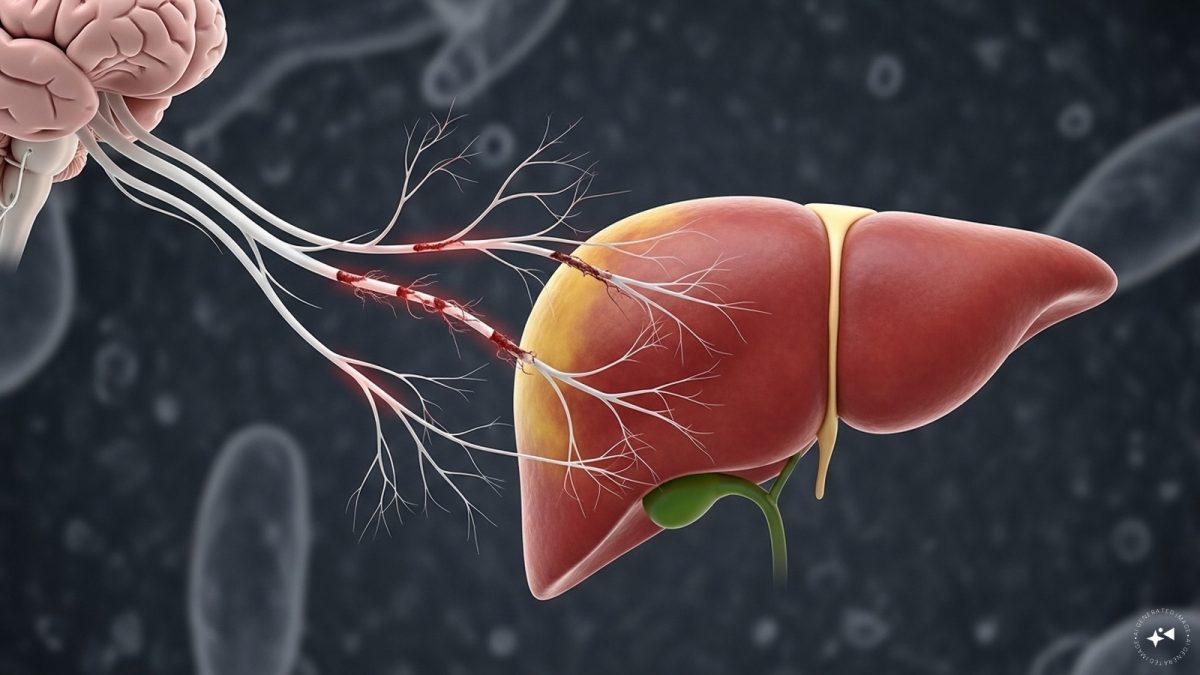
New research has unveiled a critical nexus fuelling severe weight loss or cachexia in cancer patients, a condition responsible for nearly one-third of cancer-related deaths. Scientists from the Weizmann Institute of Science and MD Anderson Cancer Center found that systemic inflammation induced by tumours disrupts the vagus nerve-mediated communication between the brain and liver.
The study noted that this disruption accelerates muscle and fat loss and worsens survival outcomes in preclinical models. It added that trials targeting this neural pathway even through noninvasive methods effectively prevented cachexia and improved responses to chemotherapy.
Medical oncologist Dr Pooja Babbar of Fortis Hospital (Manesar) said “Traditional ideas have focused on inflammation, low food intake and hormonal imbalance but this study highlights neural mechanisms. In cancer-triggered systemic inflammation, she explained, “the vagus nerve—the highway for communication between the brain and the liver—becomes dysregulated. This disrupts liver metabolism and accelerates the wasting process.”
Dr Babbar points out that cachexia affects up to 85% of patients with certain cancers, often proving resistant to conventional interventions such as solely increasing nutritional intake.
“The study demonstrates that noninvasive blockade of the right vagus nerve prevented cachexia in animal models, improving survival, health and response to chemotherapy. With these techniques already used in other clinical contexts, translation to cancer care could happen quickly if proven effective in humans,” she said.
According to Dr. Babbar, since these neuromodulation techniques are already applied clinically for other conditions, their translation into cancer therapy “may be relatively rapid.”
Dr. Pushpinder Gulia, director of surgical oncology at CK Birla Hospital (Gurugram) drew attention to how cachexia complicates cancer care, saying that weight loss is a common phenomenon,” he said.
Impact Shorts
More Shorts“Nearly 60% of lung cancer patients and approximately 80% of those with gastrointestinal or pancreaticobiliary malignancies experience unintentional weight loss.” He emphasized the multifactorial causes from poor oral intake and treatment side effects to tumour-induced metabolic disruption and warned that advanced weight loss lowers treatment tolerance, raises complication risks, and affects survival.
What is Cachexia?
Cachexia is notoriously difficult to manage in cancer care. Dr. Babbar described it as “a multifactorial syndrome with inflammation, metabolic deformity, and low appetite,” one that resists conventional interventions like nutritional support or appetite stimulants. Targeting the brain–liver vagal axis could offer the first direct intervention in the neuro-metabolic cascade behind this devastating condition.
As Dr. Gulia put it, tackling cachexia effectively could preserve treatment tolerance, enhance quality of life and potentially extend survival for those battling advanced malignancies.
With neuromodulation already in use for other clinical purposes, scientists are optimistic that clinical trials for cachexia treatments could be fast-tracked. Should these approaches prove safe and effective in humans, they may finally offer a life-altering advance against one of oncology’s most deadly and under-treated complications.
)