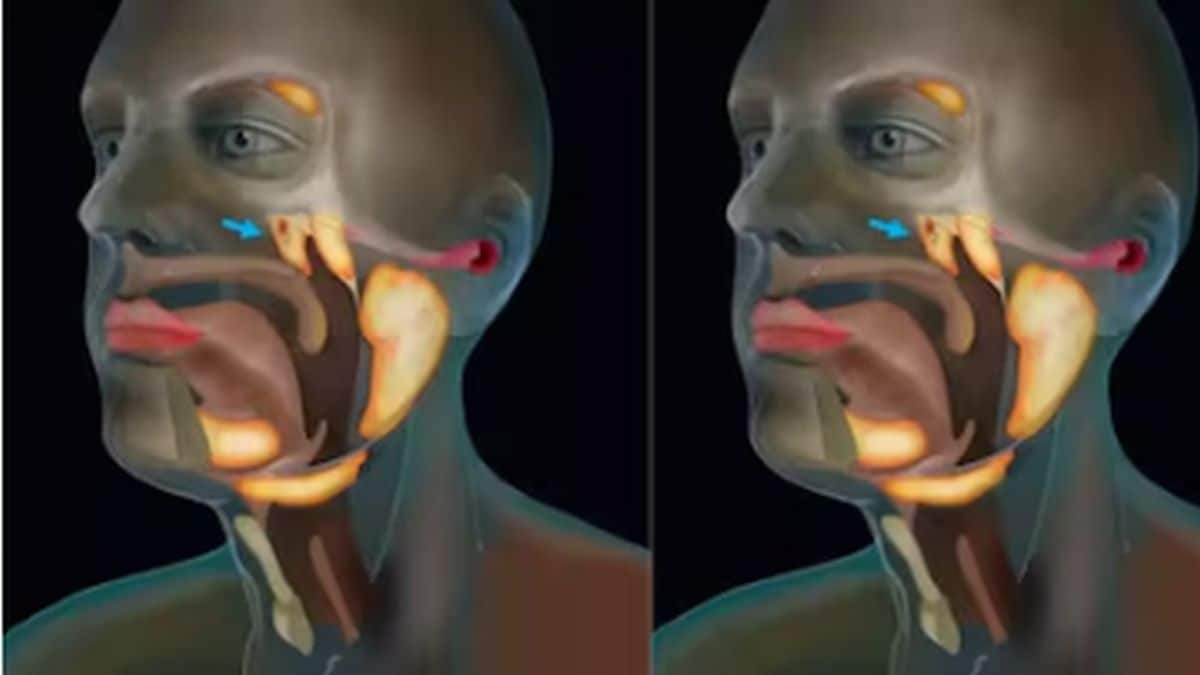
While COVID-19 is predominantly a respiratory disease, research indicates that the infection also affects other systems in the body, especially the cardiovascular, central nervous and gastrointestinal systems. A recent study published in Neurology, for example, says that COVID-19 causes neurological injuries and brain damage due to low oxygen levels or hypoxia. But even as more research is being conducted into how the COVID-19 infection affects the brain and central nervous system, which neurological symptoms show up in patients and what the long-term effects of such damage may be, studies focusing on just delirium as a symptom of COVID-19 are sparse. This indicates a major gap in our knowledge about COVID-19 which, if addressed soon, can provide better care and therapy to COVID-19 patients. Delirium and COVID-19 Delirium is defined as a serious disturbance in mental abilities which encompasses a decline in mental status, attention, cognition and consciousness of surroundings. It is a confusional state of mind, usually caused by acute changes in the brain’s function due to structural or chemical processes. Anything that affects the brain at the neurotransmitter, neuroendocrine or neuroinflammatory level can cause delirium. A June 2020 study in Acta Neurologica Belgica states that fever and hypoxia due to COVID-19 infection is likely to cause delirium in elderly patients. In others, the presence of comorbidities like hypertension, cardiovascular diseases, diabetes, hepatitis B infection, chronic obstructive pulmonary disease, chronic kidney disease and immunodeficiency can also trigger delirium. Another study, published in Age and Ageing in September 2020, concurs that delirium is a key symptom of COVID-19 in elderly patients with frailty. In fact, delirium should be treated as an early warning sign of COVID-19 in old people. Delirium as an early symptom A new study published in the Journal of Clinical Immunology and Immunotherapy suggests that delirium could present as an early warning sign of COVID-19 in not just the elderly but also in other patients, especially when accompanied by a fever. The study, conducted by researchers from University Oberta de Catalunya (UOC), was based on a systematic review of current studies on the neurological impact of COVID-19. The motive of the study was to find the pathogenic process that leads to delirium in COVID-19 patients, especially when it precedes other symptoms like coughing and respiratory difficulties and accompanies other neurological signs like loss of sense of taste or smell. The researchers identified three key factors that lead to delirium in COVID-19 patients: 1. Hypoxia: When an organ like the brain is deprived of oxygen at a tissue level, it can result in neuronal swelling and brain edema which in turn causes brain damage. Microscopic examination of brain specimens collected from patients who had died of COVID-19 show acute hypoxic injury to the brain, which is associated with neurological symptoms like delirium, anosmia and ageusia. 2. Neuronal inflammation: This brain-damaging complication occurs when the immune system is overactivated, leading to an increase in the levels of inflammatory cytokines and the overactivation of T cells. This eventually leads to cytokine storms, which can severely damage brain function. 3. Neuronal toxicity: Though rare, there are cases where the SARS-CoV-2 virus is able to directly invade the central nervous system, cross the blood-brain barrier and cause toxicity in the brain. Such toxicity leads to neuronal degeneration and neurological symptoms before the virus has even infected the lungs, leading to the presenting symptom of COVID-19 being delirium and fever instead of a cough. The study suggests that any one or all three of these factors can combine to cause delirium in COVID-19 patients by affecting key brain functions like immune-inflammatory regulation, hormonal regulation via the hypothalamic-pituitary-adrenal axis and neurotransmitter regulation. This understanding of underlying brain mechanisms in COVID-19 infection can help develop new forms of therapies that can tackle symptoms like delirium early on. The researchers conclude that though giving neurological care and medications along with treatment for COVID-19 might be difficult, screening at-risk patients for brain damage early on can help prevent long-lasting problems. For more information, read our article on Neurological symptoms of COVID-19. Health articles in Firstpost are written by myUpchar.com, India’s first and biggest resource for verified medical information. At myUpchar, researchers and journalists work with doctors to bring you information on all things health.
But even as more research is being conducted into how the COVID-19 infection affects the brain and central nervous system, which neurological symptoms show up in patients and what the long-term effects of such damage may be, studies focusing on just delirium as a symptom of COVID-19 are sparse.
Advertisement
End of Article


)
)
)
)
)
)
)
)
)



