Today, the Oxford University vaccine candidate for COVID-19 is entering clinical trials. According to the World Health Organisation’s list of 70 COVID-19 vaccine candidates, this will be the fourth COVID-19 vaccine to enter the clinical trial phase after the Moderna candidate in the USA and two others in China. The vaccine called ChAdOx1 is being worked on currently at the Jenner Institute under Oxford University by a group of researchers led by Professor Sarah Gilbert, Professor Andrew Pollard, Dr Sandy Douglas, and Professor Teresa Lambe. Professor Adrian Hill, the director of the Jenner Institute, is also leading the team. [caption id=“attachment_795429” align=“alignleft” width=“380”]  Representational image. Reuters.[/caption] However, what makes this vaccine different from its peers is the speed at which it is being prepared for mass immunisation. Dr Pollard, the chief investigator on this study has reportedly announced last week that they aim to produce about a million doses of this vaccine by Septemeber. The team already has three manufacturing partners in Britain, two in Europe, one in India and one in China. It is important to note that these doses are being prepared at a risk. Though the research team at Oxford University are very confident about the vaccine, in case the trials prove the vaccine is not effective, all these doses will go to waste. On April 21, Matt Hancock, Secretary of State for Health and Social Care, UK announced in a press briefing that this vaccine candidate for COVID-19 will be under clinical trials from Thursday, April 23, 2020. The UK government has already released massive funding for the same.
ChAdOx1
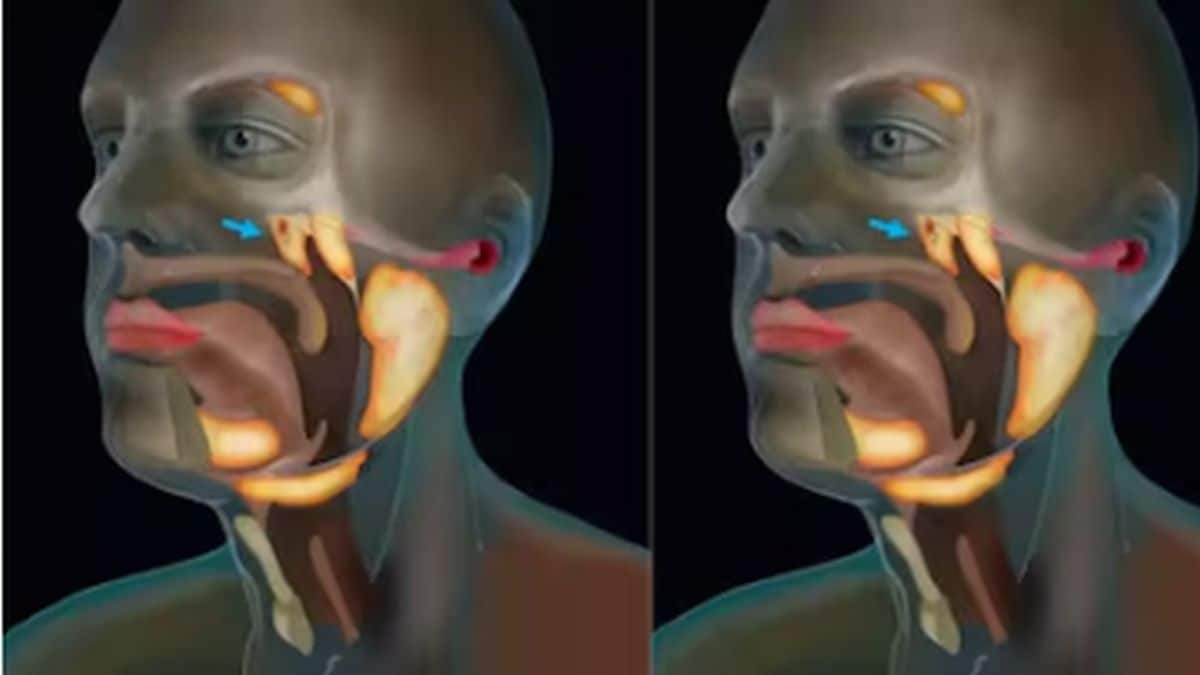
The vaccine candidate ChAdOx1 is an adenovirus vector vaccine - one of the most common types of vector vaccines. A vector vaccine uses a vector microbe - another virus/bacteria to carry the tiny piece of the nucleic acid of a harmful microbe against which immunity needs to be generated. The vector itself usually does not cause harm to the person. However, once inside the body, it produces specific proteins using that tiny piece of the nucleic acid from the harmful microbe. Our immune system identifies those proteins as if the harmful microbe has actually entered our body and starts producing antibodies against it. Hence, the person is protected from the disease without ever acquiring it. The adenovirus vector in the ChAdOx1 vaccine is reportedly using a spike protein from SARS-CoV-2 (the virus that causes COVID-19). It will not replicate inside the body and hence will be safe for children, adults, the elderly as well as those suffering from chronic diseases. According to news released by the Oxford team, they had started designing this vaccine as early as January 10, 2020. Adenovirus vaccines, in general, are well studied and have been used in 1000s of candidates in various countries in various age groups. Unlike the Moderna vaccine candidate for COVID-19, the Oxford vaccine reportedly generates a strong immune response in a single dose and hence may need lesser time to complete clinical trials. The team working on this vaccine have previously worked on the Ebola Vaccine in 2014 and have also worked on a vaccine for another coronavirus disease - Middle Eastern Respiratory Syndrome (MERS). Interestingly, the vaccine candidate from China that has entered into phase 2 clinical trials is also a type of non-replicating adenovirus vector vaccine.
The clinical trials
For the clinical trials of their vaccine, the Oxford University team started enrolling healthy volunteers in the age of 18-55 years in March and their primary outcome data is supposed to show up by May 2021. A total of 510 people will be included in the study for now and will be divided into five different study groups. All of the candidates will either get the vaccine or the control injection (which would not contain the vaccine). These trials will give information on the safety of the vaccine and the ability of the vaccine candidate to generate an immune response. According to the data from the Clinical trials registry of NIH, it will be a combined phase 1 and 2 clinical trials and will take approximately 6 months to be completed. The participants will have the option to come for an additional follow up visit after a year - 364 days to be precise. Most experts have said that a vaccine will take 12-18 months to become available for use. The scaled-up manufacturing of this vaccine could possibly shorten that timeframe if the trials are successful. For more information, read our article on WHO Solidarity Project to find a treatment for COVID-19. Health articles in Firstpost are written by myUpchar.com, India’s first and biggest resource for verified medical information. At myUpchar, researchers and journalists work with doctors to bring you information on all things health.


)
)
)
)
)
)
)
)
)



